You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Computer-aided design (CAD) and computer-aided manufacturing (CAM) have become an increasingly popular part of dentistry over the last 25 years. CAD/CAM technology was developed to address three challenges. The first challenge was to ensure adequate strength of the restoration, especially for posterior teeth. The second challenge was to create restorations with a natural appearance. The third challenge was to make tooth restoration easier, faster, and more accurate. In some cases, CAD/CAM technology provides patients with same-day restorations. CAD/CAM systems are becoming increasingly popular in dental offices. In 2016, it was reported that more than 30,000 dentists around the world own scanning and milling machines, more than 10,000 of which were in the United States and Canada.1 With the popularity of CAD/CAM increasing, these numbers are certainly growing.
Historical Perspective
The revolution of digital dentistry began in 1988, when Francois Duret (the first in the field of dental CAD/CAM development) published his first article about CAD/CAM dentistry in The Journal of the American Dental Association. Disagreeing with the age-old lost wax technique, he wrote, "Regardless of the advanced state of this 300-year-old technique, information must still be transferred by hand from the impression to the finished crown via a series of materials, each of which may induce error in the final castings. This system of casting does not allow us to take advantage of tremendous advances in computers and robotics. For these reasons, we introduced CAD-CAM technologies to the dental profession in 1971."2 As time has moved forward, the software and hardware have become smaller, more reliable, and more user-friendly, allowing laboratories and dental offices to make a huge leap into the digital age-not only creating restorations, but also diagnosing and planning smile design, implant placement, orthodontic tooth realignment, and bite therapy. These changes have allowed dentists, technicians, and often patients to communicate and collaborate in real time to satisfy emotional and clinical needs in a more efficient and effective manner.
Evolving Ceramic Materials
Traditionally, many dental restorations have been milled as ceramics with great success, especially with lithium disilicate. After a mean observation time of 46 months, Reich et al (2014) recorded the CAD/CAM-generated lithium-disilicate failure-free rate and complication-free rate at 93% and 83%, respectively.3 The clinical performance of the crowns was exactly as satisfying.4
Due to the need to mill longer and stain/glaze ceramics in a firing oven, newer materials have come to the marketplace that are classified as "nanoceramics," an integration of nanotechnology and ceramics. Nanoceramic particles are milled to exacting standards. The standards are crucial because when particles vary widely in size, uncontrolled agglomeration of powders due to attractive van der Waals forces can give rise to microstructural inhomogeneities. These uneven areas yield to stresses that can lead to crack propagation. Therefore, these precise newer materials avoid uneven areas of stress and are highly durable. In tests evaluating the fracture resistance of these materials, they showed a higher fracture resistance at thicknesses less than 0.5 mm versus all-ceramic restorations.5 To summarize, these newer products offer exceptional strength for multiple situations; excellent esthetics; faster milling time; repairability if needed; less marginal chipping; and an easier material to finish.
Hybrid Ceramics
Recently, a hybrid ceramic (HC) system was created that offers even further improved physical properties for strength and esthetics.6 The new material has the following characteristics:
Composed of 61% zirconium silicate, a densely packed nanofiller forming a skeleton that uniformly absorbs masticatory forces and promotes resistance to breakdown phenomena.
Durable machinability in milling time, damage tolerance, wear of milling instruments, and the ability to be fabricated in a very low thickness.
The high flexural strength of 191 MPa and Vickers hardness of 66 Hv0.2 make the HC material a good candidate for both anterior and posterior restorations, implant-supported cases, and long-term provisionals.
The hardness of the material demonstrates values closer to dentin; thus, no excessive antagonist wear can be observed, which is a concern when using esthetic and high-strength ceramics.
Universal indications: anterior/posterior crowns, inlays/onlays, veneers
Bisphenol A (BPA)-free
Esthetics with fluorescence in four options: low translucency (posterior teeth); high translucency (inlays/anterior crowns); enamel (veneers); and two-layered (challenging anterior layered restorations).
The following is a case in which the HC material was used in a block to restore an endodontically involved tooth in a seamless and natural manner.
Case Presentation
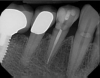
A 71-year-old man presented with acute pain in tooth No. 29 that was spontaneous, unresponsive to vitality testing, and sensitive to percussion. He was referred to an endodontist for treatment of acute apical periodontitis due to the non-vitality of the nerve. Because of the multiple restorations and lingual decay of the tooth, enamel and dentin were compromised, causing the tooth to be biomechanically at high risk and requiring an eventual post-and-core and crown (Figure 1 and Figure 2). Endodontic care included nonsurgical intracanal therapy and creating room for a post space.
CAD/CAM dentistry is very precise. For accuracy, the preoperative, shade, bite, and upper/lower tooth scans are best taken before anesthesia and dental procedures that induce muscle fatigue (Figure 3). After infiltration anesthesia with 1 carpule of articaine hydrochloride 4% and epinephrine 1:100,000 injection, the temporary was removed. Occlusal reduction of 2.0 mm was precise and defined with an 828Y depth cutting bur to meet restorative requirements (Figure 4), and the post space was restored. Axial reduction and shoulder margination were performed with a coarse KS1 bur. After smoothing of the preparation, a 15% aluminum chloride topical gingival retraction paste was injected and compressed into the sulcus, then thoroughly rinsed with water and air-dried, before scanning of the tooth preparation and critical adjacent anatomy (Figure 5 and Figure 6).
In digital dentistry, excellent margination is possible, with magnification and without potential dimensional distortion caused by analog impression taking, pouring models, and trimming dies with the historical methods (Figure 7). Restorative design was performed by the assistant by visualizing the axis of draw, the adjacent contact areas, and occlusal harmony in centric occlusion using the "bio-individual" mode in the software. When complete, the design was confirmed and approved by the restorative dentist (Figure 8). Milling of the HC block was done in a milling unit that cut external and internal anatomy of the new restoration. The HC block can be milled 3 to 4 minutes faster than lithium disilicate and can be taken to the mouth for adjusting, polishing and/or custom staining without the need for crystallization for strengthening or glazing. For this restoration, the author chose to do a combination of polishing, staining, and glazing with material-specific items for maximum gloss and esthetics.
After the sprue was removed, the contacts and occlusion were refined with a green stone so the crown was seated accurately and comfortably for the patient. These vectors are calibrated with the machine, so adjustments can be kept to a minimum. Smoothing the occlusal/gingival half was performed with a point, followed by a buff wheel polish using aluminum oxide paste, creating a nice gloss before tinting (Figure 9 and Figure 10). The restoration was cleaned with alcohol. While the restoration was held with a crown holder, a ceramic resin bond was thinly applied to the outside and left for 10 seconds, followed by a second resin bond in the same manner, and then light-cured for 20 seconds. Occlusal tinting with a brown stain was subtly applied with a #15 endodontic file and a thin layer placed gingivally for natural color stratification, followed by a 30-second light-cure (Figure 11).
The final external surface step in creating the crown was applying an external glaze and light-curing for 30 seconds (Figure 12). Internally the crown surface was sandblasted evenly with aluminum oxide (particle sizes 50 to 100 μm) with a pressure of 2 to 3 bars for 10 seconds. Finally, the crown was rinsed with water and dried, and a thin layer of primer was applied and light-cured for 10 seconds using a light-emitting diode (LED) light. The crown was placed under an amber-colored shield for protection (Figure 13).
Bonding the restoration requires a meticulous process to achieve success. Isolation from salivary and gingival fluids is a must. Isolation by rubber dam or a similar product is essential. Crevicular fluid must kept under control to avoid contamination. In addition, the dentin of the preparation was treated and rinsed with 2.0% chlorhexidine gluconate to remove any debris (Figure 14 and Figure 15). Selective etching of the enamel with 35% phosphoric acid for 15 seconds was followed by thorough rinsing with water. Final cementation was performed using a dual-mix translucent formulation containing primer, adhesive, and cement. The cement had an unlimited working time and 100% polymerization, and it completely light-cured in 40 seconds. Final marginal cleanup was easily performed with a carbide ET9 12-fluted bur. The patient was pleased with the convenience and esthetic results (Figure 16).
Conclusion
CAD/CAM has made dentistry a better experience for patients. Restorations through CAD/CAM require fewer visits and are less cumbersome, eliminating bulky impressions and the need to wear a temporary restoration. Dental manufacturers are improving efficiency and effectiveness with products that are strong and innovative. The future continues to appear promising for dental patients and professionals.
About the Author
Hugh Flax, DDS
Private Practice
Atlanta, Georgia
References
1.Phat N. The use of CAD/CAM in dentistry. Pocket Dentistry. https://pocketdentistry.com/the-use-of-cadcam-in-dentistry/. Published October 9, 2016. Accessed August 15, 2018.
2.Duret F, Blouin JL, Duret B. CAD-CAM in dentistry. J Am Dent Assoc. 1988;117(6):715-720.
3. Reich S, Endres L, Weber C, et al. Three-unit CAD/CAM-generated lithium disilicate FDPs after a mean observation time of 46 months. Clin Oral Investig. 2014;18(9):2171-2178.
4.Reich S, Schierz O. Chair-side generated posterior lithium disilicate crowns after 4 years. Clin Oral Investig. 2013;17(7):1765-1772.
5.Chen C, Trindade FZ, de Jager N, et al. The fracture resistance of a CAD/CAM resin nano ceramic (RNC) and a CAD ceramic at different thicknesses. Dent Mater. 2014;30(9):954-962.
6. Ceramics & CAD/CAM. Shofu. http://www.shofu.com/en/products/ceramics-dentures/new/shofu-block-disk-hc/. Accessed August 15, 2018.